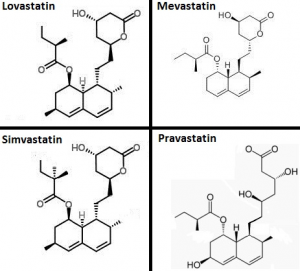
Statin medications, also known as HMG-CoA reductase inhibitors, have a good record at reducing high cholesterol levels. However, statin medications inhibit not only the body’s synthesis of cholesterol but also the body’s synthesis of Coenzyme Q10, which the heart muscle cells need for energy production and antioxidant protection. Statin drugs lower the plasma and tissue levels Coenzyme Q10. We need greater awareness of this relationship between statin drugs and the essential bio-nutrient Coenzyme Q10.
Statin medications? What are we to think? Statins undoubtedly lower cholesterol levels and reduce the number of heart attacks.
But statin medications can and do have adverse effects [Okuyama]. One of the undesirable unintended consequences of taking a statin medication is that the patient’s bio-synthesis of Coenzyme Q10 is also inhibited. The body produces cholesterol and Coenzyme Q10 in the same biological pathway. Cut off one, and you cut off the other as well.
The heart muscle cells need Coenzyme Q10
Low plasma and tissue concentrations of Coenzyme Q10 are clearly associated with increased risk of heart failure [Folkers].
Low plasma Coenzyme Q10 levels are an independent predictor of death from heart failure [Molyneux].
Note: The American Heart Association defines heart failure is the chronic, progressive failure of the heart to pump adequate quantities of blood to deliver oxygen and nutrients to the bodily organs.
Statin medication plus Coenzyme Q10 supplementation
Dr. Daniel Pella and a team of researchers at the Medical Faculty of P. J. Safarik University in Kosice, Slovakia, have investigated the effect of adding Coenzyme Q10 and/or omega-3 fatty acid supplements to the diet of heart disease patients taking a statin medication [Tóth].
Dr. Pella was also one of the researchers on the 2014 Q-Symbio study of the effect of Coenzyme Q10 adjuvant treatment in chronic heart failure [Mortensen].
In this current study, the Slovak researchers were particularly interested in studying the effect of Coenzyme Q10 supplementation on atherogenesis (= the accumulation of plaque on the inside walls of arteries).
Study design: Coenzyme Q10 and statin medications
The researchers enrolled 105 patients diagnosed with elevated cholesterol levels and elevated triglyceride levels and randomly assigned them to one of three groups.
They called the group that got the statin medication only the control group. They formed two experimental groups as follows:
- The second group got 2.52 grams of omega-3 polyunsaturated fatty acid supplements daily.
- The third group got 2.52 grams of omega-3 polyunsaturated fatty acids daily plus 200 milligrams of Coenzyme Q10 daily.
The researchers evaluated the patients at the start of the study and again at the end of the 3-month study period [Tóth].
Study results: Coenzyme Q10 and statin medications
Compared to patients in the control group, patients in both treatment groups had statistically significant reductions:
- in liver enzyme activity
- in systolic blood pressure
- in bio-markers for inflammation
- in triglyceride levels
Furthermore, the patients in the two treatment groups had significantly increased antioxidant activity:
- superoxide dismutase antioxidant activity
- glutathione peroxidase antioxidant activity
Increased health benefits with Coenzyme Q10 added
Now comes the most gratifying aspect of the research study. The combination of Coenzyme Q10 supplementation and polyunsaturated fatty acids, added to the statin medication, significantly reduced important parameters even beyond what adding the omega-3 fatty acids alone did:
- reduced systolic blood pressure
- reduced hsCRP – a bio-marker for inflammation
- reduced IL-6 – a bio-marker for inflammation
Coenzyme Q10 and superoxide dismutase levels
The addition of the daily Coenzyme Q10 supplements further improved the activity of the very important antioxidant called superoxide dismutase. Superoxide dismutase and glutathione peroxidase are the most important antioxidant enzymes protecting the cells and lipids and proteins and DNA against oxidative damage caused by harmful free radicals.
Coenzyme Q10 and fewer adverse effects of statins
Moreover, the addition of the Coenzyme Q10 to the treatment significantly reduced the intensity of the adverse effects of the statin medication.
Conclusion
This is an important study [Tóth]. The addition of omega-3 fatty acid supplements and Coenzyme Q10 supplements to the diet of patients taking statin medications confers beneficial health effects related to atherogenesis and side effects of statin treatment.
The Coenzyme Q10 preparation used in this study is the same Coenzyme Q10 supplement used in the following studies:
- Q-Symbio study [Mortensen 2014]
- KiSel-10 study [Alehagen 2013]
- Gulf War Veterans study [Golomb 2013]
Sources
Alehagen, U., Johansson, P., Björnstedt, M., Rosén, A., & Dahlström, U. (2013). Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and Coenzyme Q10 supplementation: a 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. International Journal of Cardiology, 167(5), 1860-1866.
Folkers, K., Vadhanavikit, S., & Mortensen, S. A. (1985). Biochemical rationale and myocardial tissue data on the effective therapy of cardiomyopathy with Coenzyme Q10. Proceedings of The National Academy of Sciences of The United States of America, 82(3), 901-904.
Golomb, B. (2014). Coenzyme Q10 and Gulf War illness. Neural Computation, 26(11), 2594-651.
Molyneux, S. L., Florkowski, C. M., George, P. M., Pilbrow, A. P., Frampton, C. M., Lever, M., & Richards, A. M. (2008). Coenzyme Q10: an independent predictor of mortality in chronic heart failure. Journal of The American College of Cardiology, 52(18), 1435-1441. doi:10.1016/j.jacc.2008.07.044
Mortensen, S. A., Rosenfeldt, F., Kumar, A., Dolliner, P., Filipiak, K. J., Pella, D., & Littarru, G. P. (2014). The effect of Coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC. Heart Failure, 2(6), 641-649.
Okuyama, H., Langsjoen, P. H., Hamazaki, T., Ogushi, Y., Hama, R., Kobayashi, T., & Uchino, H. (2015). Statins stimulate atherosclerosis and heart failure: pharmacological mechanisms. Expert Review of Clinical Pharmacology, 8(2), 189-199. doi:10.1586/17512433.2015.1011125
Tóth, Š., Šajty, M., Pekárová, T., Mughees, A., Štefanič, P., Katz, M., & … Pella, D. (2017). Addition of omega-3 fatty acid and coenzyme Q10 to statin therapy in patients with combined dyslipidemia. Journal of Basic and Clinical Physiology and Pharmacology, 28(4), 327-336. doi:10.1515/jbcpp-2016-0149
The information presented in this review article is not intended as medical advice and should not be used as such.








Leave A Comment